Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Diagnostics
Covid-19
Can breath tests sniff out COVID-19?
Breath-based diagnostics may provide a quicker and cheaper way to diagnose SARS-CoV-2 infections
by Carrie Arnold, special to C&EN
September 21, 2021
| A version of this story appeared in
Volume 99, Issue 35

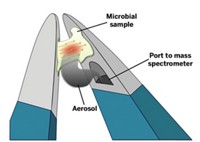
Drivers crossing into Singapore at the Tuas Checkpoint have always had to show their passports or work visas. Since May, however, the 200,000 daily travelers have also had to provide a different kind of information: the molecular makeup of their breath. Each driver rolls down their window and exhales into a large, disposable, cigar-sized mouthpiece connected to a mass spectrometer. In less than 60 s, their breath sample is analyzed to determine whether they have COVID-19.
Support nonprofit science journalism
C&EN has made this story and all of its coverage of the coronavirus epidemic freely available during the outbreak to keep the public informed. To support us:
Donate Join Subscribe
This breath test, developed by Singapore-based Breathonix, is an alternative to the many COVID-19 tests that require going spelunking through someone’s nasal passages with a long cotton swab.
Infection with the virus SARS-CoV-2 triggers a series of metabolic changes that alter the ratios of volatile organic compounds (VOCs) in exhaled breath. The raised or lowered levels of compounds such as acetone and undecanal can determine if someone has an infection and what pathogen might be causing it—or so the theory goes. Companies including Breathonix, Israel’s Scentech Medical and TeraGroup, and Owlstone Medical in the UK have all launched Breathalyzer-like tests to detect COVID-19. And researchers in Indonesia have created a COVID-19 breath test called GeNose C19. Breath tests are especially useful for mass-screening opportunities at large public events and border crossings berrcause of their speed and low cost, according to Paul Thomas, director of the Centre for Analytical Science at Loughborough University.
But some question whether the technology is sensitive enough. Diagnosing COVID-19 requires measuring how much the VOCs in someone’s breath deviate from the norm, but researchers have yet to define the levels of these compounds in the breath of healthy people. These concerns were driven home when the Dutch government halted use of a device called SpiroNose, developed by the Netherlands-based Breathomix, at several testing sites around Amsterdam after just a few days. A non-peer-reviewed article published in February initially looked promising: SpiroNose distinguished between 35 samples from people who tested positive for COVID-19 via polymerase chain reaction (PCR) and the 869 who were negative. But real-life findings were more disappointing. In the first few days of its use by public health officials, the SpiroNose failed to detect infection in 25 individuals, some of whom were ultimately hospitalized. In media statements, Breathomix attributed the discrepancies to user error.
Still, breath-based diagnostics are probably here to stay.
“It has the potential to serve as a replacement for highly invasive tests,” says Oliver Gould, a chemistry research associate at the University of the West of England (UWE), Bristol. “Replace those with a breath sample, and uptake will be superior.”

Building a breath test
For thousands of years, astute physicians have used breath to diagnose medical conditions. Different diseases cause different metabolic changes, some of which are characteristic enough to be detected by the human nose. The ketones produced when someone with diabetes must metabolize fatty acids for energy make breath smell like nail polish remover. Liver failure gives breath the odor of musty fish (from dimethyl disulfide and methyl mercaptan), and cultures of Pseudomonas aeruginosa often smell like grape juice because the bacterium produces 2-aminoacetophenone.
But “take two whiffs and call me in the morning” is hardly a precise method of diagnosis. The first breath-based tests trace back to the 1930s in the US, when skyrocketing car ownership coincided with the end of Prohibition. Drunk driving was suddenly a major problem, and law enforcement needed a way to establish that someone was intoxicated. Enter Emil Bogen’s simple breath test. A driver could exhale into the leather bladder of an American football containing sulfuric acid and potassium dichromate. If they had been drinking, the mixture would change from yellow to various shades of blue green. But his test was bulky and impractical for use at traffic stops. Other inventions came along, culminating in 1954 with forensic scientist Robert Borkenstein’s Breathalyzer. The portable device uses two electrodes to measure the electrical current produced by the oxidation of ethanol to acetic acid at the anode and the reduction of oxygen to water at the cathode. The device’s portability, accuracy, and ease of use by nonscientists mean that Borkenstein’s Breathalyzer is now used by police around the world to test drivers in the field.
The success of the Breathalyzer spurred interest in breath-based diagnostics for medicine. In a 1982 Nature paper, a pair of chemists at the University of Warwick were the first to propose the idea of an electronic nose, which would use an array of chemical sensors to detect the molecular fingerprint of a specific odor, much like the human olfactory system. Around that same time, improvements in gas chromatography/mass spectrometry were making it easier to detect minuscule traces of molecules. And because the VOCs in someone’s breath reflect the person’s underlying metabolism, scientists deduced that they should be able to link specific changes in this chemical profile to specific diseases. If service dogs could detect hypoglycemia in someone with diabetes, researchers reasoned, these changes had to be chemical in nature, which meant they could be measured.
From the outset, scientists have struggled to determine whether and how a condition changes breath VOCs and nonvolatile breath biomarkers. Cristina Davis, an interdisciplinary engineer at the University of California, Davis, says that VOC shifts are often the same across several conditions. “You could have the same compounds increasing in lung cancer as you do with a sprained ankle or bacterial infection,” says Jonathan Beauchamp, manager of the Emissions Analytics and Diagnostics group at the Fraunhofer Institute for Process Engineering and Packaging IVV in Freising, Germany.
But many conditions do generate a unique pattern or relative ratio of breath biomarkers. Scientists believe most diseases shift the amounts of VOCs normally present in someone’s breath, increasing some while lowering others. To work as a diagnostic, then, a system needs to identify the presence of a molecule, measure its level, and compare that level with the levels of other chemicals present in breath, Davis explains. Building a breath-based diagnostic would require scientists to measure a typical profile of VOCs in breath and account for the environment’s strong effect on what we breathe.

Measuring molecular signatures
Twenty thousand times each day, we exhale. Air leaves our lungs like water being wrung from a sponge: the air that’s near the surface exits first, followed by the gases deeper in our respiratory tracts. That first part of our breath, says Audrey Odom John, chief of infectious diseases at Children’s Hospital of Philadelphia (CHOP), is known as mixed exhaled air, and it comes from the bronchiral tree and upper part of the lung. It also contains pungent odors, such as those from morning breath or a recent meal.
The last air to exit is the end-exhaled air. That’s the bit that contains “the nectar with the information” that diagnostic companies are chasing, Loughborough University’s Thomas says. It comes from the lower alveoli, where gas exchange happens and VOCs made by our bodies mix with the air we are about to exhale. This exhaled air also carries saliva, creating what’s known as exhaled breath condensate, in which some of the exhaled VOCs are dissolved. In total, each exhaled breath carries varying amounts of more than 250 compounds, the levels of which can change according to age, sex, time of day, environment, and disease state. Because of this variability, clinical trials on breath biomarkers require hundreds, even thousands, of participants, Davis says.
Because those hundreds of VOCs are present in minute quantities, scientists need to concentrate the molecules—usually by cooling and condensing the exhaled breath condensate or passing the collected breath over a sorbent. Mass spectrometry remains the gold standard for analyzing those concentrated samples, Davis says. “These [machines] are what we use to figure out, ‘OK, what’s the identity of these suckers in the fingerprint?’ ”
But mass spec machines carry a high price tag and are too big to be used in the many settings where you’d want to do rapid testing. Singapore’s Breathonix has gotten around the problem by situating the mass spectrometer on-site and using the steady flow of traffic through the Tuas Checkpoint to make the investment worthwhile. The University of Miami is using a similar strategy in a study of a COVID-19 breath test developed by the diagnostics firm TeraGroup. The company’s proprietary breath analysis machine uses high-frequency terahertz electromagnetic waves to detect the spectral signature of VOCs associated with SARS-CoV-2 infection. The university set up the equipment in a temperature-controlled building on campus, according to Roy Weiss, chair of the Department of Medicine at the university’s Miller School of Medicine and chief medical officer for the university’s COVID-19 response. Davis has also seen a lot of interest in portable ion mobility spectrometry and gas chromatography systems because they are smaller than traditional mass specs and can operate in a variety of conditions.
During the H1N1 influenza pandemic, scientists determined that many of the common changes they were detecting in breath VOCs were a result of the host’s immune response—for example, 2,3-butanedione, 2,8-dimethylundecane, and n-propyl acetate. But scientists didn’t know whether different viral infections would lead to different VOC signatures. Even if a breath test couldn’t identify the specific virus causing symptoms, a test that could differentiate between viral and bacterial infections would still be extremely valuable, UWE Bristol’s Gould says.
“It doesn’t really sound like it’s that important, but actually it really is when we’re talking about antibiotic resistance and ensuring that patients are put on the correct treatment as rapidly as possible,” Gould says.
The current pandemic has made distinguishing between COVID-19, influenza, or a more harmless respiratory infection crucial. To find molecules in breath that could be a unique signature of COVID-19, scientists dug deep into the chemical cascade that occurs once a virus infects the body, a process that includes a burst of free radicals and an increase in fatty acid metabolism to fuel immune activity. Their first task was to determine whether COVID-19 changed a person’s breath profile and whether these changes were different from those caused by other viral infections.
Early in the pandemic, Peking University’s Maosheng Yao and colleagues found that hospitalized patients with COVID-19 breathed out more ethyl butanoate than people with non-COVID-19 respiratory infections, whereas people with non-COVID-19 respiratory infections had higher levels of butyraldehyde and isopropyl alcohol. This work was posted to the preprint server medRxiv and thus did not undergo peer review.
“All of these changes form a unique pattern. We found a fingerprint of 12 key compounds,” Yao says.
Around the same time, Loughborough’s Thomas, along with collaborators in Germany, used gas chromatography/ion mobility spectrometry to analyze breath samples in hospitalized COVID-19 patients. In a December 2020 study in EClinicalMedicine, the team found that the presence of aldehydes (ethanal, octanal, and heptanal), ketones (acetone and butanone), and methanol distinguished COVID-19 patients from those with other respiratory diseases. The test had greater than 82% sensitivity and 75% specificity, Thomas says, noting that the team is on the right track but that the diagnostic still needs improvement. Breathonix’s test, by comparison, has 97% specificity and 85.5% sensitivity, according to the company’s data. Those levels are on par with those of PCR tests.
What makes breath-based testing even more valuable than PCR and antigen tests for SARS-CoV-2 is that scientists might be able to detect VOC changes before a person begins shedding the virus, which Yao says could help reduce disease spread. CHOP’s Odom John is conducting clinical trials to determine whether people’s breath profiles change during infection. That knowledge could potentially allow researchers to link VOCs to both infection and infectiousness. Owlstone Medical is also working on a breath-based test to help diagnose lung damage in people recovering from COVID-19.
Advertisement
But some in the breath research field worry that scientists don’t yet know enough about how to distinguish between COVID-19 and other viral infections to launch large-scale testing programs. Especially after the high-profile false negatives obtained by the SpiroNose, researchers around the world are watching Singapore’s use of the breath tests with interest—and trepidation. This uncertainty hasn’t slowed the hype, according to Owlstone’s CEO, Billy Boyle. Many advancements are being dangerously oversold in the media. What the field really needs, he says, “is less PR and more papers.”
As the Delta variant has swept around the world, the need for rapid testing is perhaps more important than ever before, the University of Miami’s Weiss says. Breath testing’s low cost and rapid turnaround make it perfectly poised to fill a crucial niche. “It has the potential to really change pandemic response,” he says.
Fraunhofer IVV’s Beauchamp says he has no doubt that breath tests will eventually become common medical practice, just as urine and blood tests are. But first, scientists will need to finish the long slog of standardization and validation. Few studies have been replicated, a critical step in creating a robust diagnostic. “This lack of reproducibility across labs is a big challenge,” Beauchamp says.
Despite the challenges facing breath research, Thomas says the pandemic has transformed the field from a relative scientific backwater with a handful of researchers into a multimillion-dollar juggernaut on the cutting edge of medical science. When the field’s scientists focused on the COVID-19 problem together, they were able to make progress in just weeks, Thomas says. “For me, that is a definite statement about the potential of this as a diagnostic approach.”
Carrie Arnold is a freelance public health reporter based in Virginia.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter